The Influence of Body Position on the Blood Flow of Parenchymatous Organs: II. Kidneys
Human Physiology. Vol. 25. No. 2. 1999. pp. 203-209. Translated from Fiziologiya Cheloveka, Vol. 25, No. 2. 1999. pp. 92-98. Original Russian Text Copyright © 1998 by Minvaleev, Kuznetsov, Nozdrachev.
The Influence of Body Position on the Blood Flow of Parenchymatous Organs: II. Kidneys
R. S. Minvaleev, A. A. Kuznetsov and A. D. Nozdrachev
Received May 14,1998
Abstract—The influence of yoga exercise known as bhujangasana or the cobra position on the systemic and intrarenal blood flow was studied in three stages of experiments in healthy subjects of both sexes (the mean age of 36.2 years) byduplex ultrasound dopplerography with colored mapping of the blood flow. During exercise, cardiac output into the ascending aorta decreased in all subjects (n = 10), the pulse blood flow in the interlobular renal arteries (n = 9) decreased, and the minute blood flow remained stable. The outflow in the renal vein (n = 22) at the level of the renal hilum significantly increased during right-atrial systole up to full flattening of the velocity spectrum. According to the preliminary data, exercise in the cobra position helped restore normal pulsations of the disturbed renal monophase venous blood flow.
To continue our earlier studies of the influence of hatha yoga positions on the intraorgan blood flow [1], we have chosen kidneys as a parenchymatous organ involved in homeostasis. Our choice was also based on the reports that the cobra position (bhujangasana in Sanscrit) had an influence on the renal state and function [2] (Fig. 1).

Fig.1. Cobra position known in yoga exercises as bhujangasana
Note: This position appears as the vertebral column flexure when lying on one’s belly without supporting oneself by the arms. Unlike the usual flexure backwards, the correct performance of bhujangasana should be characterized by the efforts to cave in the (inflexible!) vertebral region. And only such a performance preconditions a correct reproducibility of our data on hemodynamic parameters in this position.
MATERIALS AND METHODS
The work was performed in three stages. The first stage included the study on nine subjects (including seven women) aged from 20 to 45 (32.1 years on average) who had been taught to perform exercise in the cobra position. Using a HITACHI Eub-565 echo-chamber (Japan), blood flow in the interlobular arteries of the left kidney was recorded before exercise, during its performance, and immediately after it. The following parameters were determined: the maximum flow velocity (Vmax, cm/s): the medium flow velocity (Vmed, cm/s); the flow velocity integral per one cardiac cycle and per minute (FVI and Flow, cm and cm/min, respectively); the pulse and resistive indices (PI and Rl, respectively, conventional units) describing the muscular activity of the arterial wall; and the heart rate (HR, beats/min).
In the second stage, blood flow in the ascending aorta was determined from the retrostemal approach during exercise in ten subjects (eight of them were women between the ages of 20 and 50, 32.4 years on average). In this case, only the index of flow velocity integral per minute was recorded, which was calculated by the formula Flow/BSA = FVI x HR/BSA (cm/min m2) where BSA is the body surface area. In this work, we have abandoned the traditional calculation of aortal flow volume because of difficulties in the measurement of its diameter. Under these conditions, it would be improper to compare the central hemodynamics in different subjects; therefore, we followed changes in the flow velocity integral separately in each subject under study. We acknowledged that the aortal diameter should be unchangeable as the diameter of a rigid elastic vessel.
In the third stage, the influence of the exercise on the venous outflow from the kidney was determined. A controlled volume of the Doppler signal was placed into the renal vein at the level of renal hilum at the initial horizontal position on the belly, during exercise, and at the horizontal position immediately after it. This examination was carried out in 22 subjects (including 14 women, aged from 26 to 63, 41.7 years on average). The central and venous hemodynamics were studied with a KONTRON Sigma-44 echo-chamber (France). The venous outflow was assessed according to changes in flow velocity during right-ventricular systole (VS, cm/s) and right-atrial systole (VA, cm/s) (Fig. 2); the heart rate (HR, beats/min) was also recorded.
When discussing the results, we also considered our clinical observations on the venous renal outflow in patients with some renal diseases. Some of these studies were carried out with Sinergy and System Five echo chambers (Vingmed, Norway). These echo-chambers were available for our studies thanks to the employees of the St. Petersburg branch of VINGMED-SONOTRON, and we are grateful to them.
The results were statistically treated using a STATGRAPHICS packet of applied programs, and the significance of changes was evaluated with Student’s t-test for coupled samples.
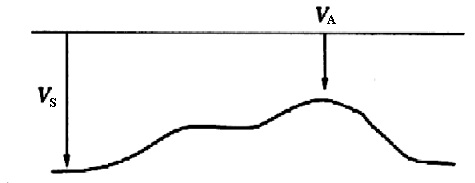
Fig. 2. Scheme of normal blood flow in the renal vein.
RESULTS
The initial parameters of blood flow in the interlobular renal arteries in test patients were similar to values published for healthy subjects [3]. The maximal and average flow velocities were 0.28±0.01 and 0.17±0.01 cm/s, respectively: FVI and Flow were 0.16± 0.01 and 10.0±0.6 cm, respectively; PI was 1.12±0.05 c.u., and RI was 0.67±0.01 c.u. The initial heart rate (HR) was 62.8±1.0 beats/min. During exercise, HR sharply increased (up to 106±4.6 beats/min, p<0.001), the velocity integral of one pulse wave FVI considerably decreased to (0.10±0.01 cm, p<0.01), whereas the flow velocity integral per minute (Flow) did not change (10.0±0.07, p<0.05). Other parameters were stable. After the exercise, all parameters did not differ from those observed initially (Table 1).
The parameters of venous outflow from the kidney (Table 2 and Fig. 3) indicated that during exercise the flow velocity in the renal vein in the right-ventricular systole, VS did not change (-14.4±1.4 and -16.0±1.8 cm/s, p<0.05), whereas the outflow in atrial systole, VA, significantly increased (from -4.5±1.4 to -10.2±1.2 cm/s, p<0.01). The heart rate increased from 78.5±2.9 to 112.8±4.3 beats/min, p<0.001). After exercise, these parameters were restored to their initial values.
Changes in the index of flow integral in the ascending aorta (Flow/BSA, cm/min m2) seemed to be similar to the cardiac index. During exercise, this parameter decreased in all test subjects (Fig. 4). Based on this observation, it was suggested that the stroke volume of the left ventricle decreased so markedly during exercise that the minute flow volume significantly decreased, despite the development of tachycardia (Fig. 5).
DISCUSSION
It seems that the significantly decreased pulse filling in the interlobular renal arteries (FVI) observed during exercise was compensated for by increased heart rate until the minute organ blood filling (Flow) was stable. This occurred along with decreased minute general blood flow because of the sharp fall of the left-ventricular beat. Thus, exercise-induced redistribution of arterial blood in favor of kidneys was suggested.
Table 1. Changes in the parameters of renal arterial inflow in the cobra position (n = 9)
|
Parameters |
Initially |
Position |
After the exercise |
||
|
|
X ± m |
X ± m |
p |
X ± m, |
p |
Vmax, cm/s |
0.28 ± 0.01 |
0.26 ± 0.02 |
n/d |
0.31 ±0.02 |
n/d |
|
Vmed, cm/s |
0.17±0.01 |
0.17±0.01 |
n/d |
0.18±0.01 |
n/d |
|
FVI. cm |
0. 16 ± 0.01 |
0.10±0.01 |
** |
0.1 8 ± 0.01 |
n/d |
|
Flow, cm/min |
10.0 ± 0.6 |
10.0 ± 0.7 |
n/d |
10.9 ± 0.6 |
n/d |
|
PI, c.u. |
1.12 ± 0.05 |
0.98 ± 0.06 |
n/d |
1.13 ± 0.06 |
n/d |
|
RI, c.u. |
0.67 ± 0.01 |
0.62 ± 0.02 |
n/d |
0.67 ± 0.02 |
n/d |
|
HR, beats/min |
62.8 ± 1.0 |
106.0 ± 4.6 |
** |
61.4± 1.6 |
n/d |
Note: Here and in Table 2: n/d, diflerences are absent. * p <0.01. **p <0.001.
Table 2. Changes in the parameters of renal venous outflow in the cobra position (n = 22)
|
Parameters |
Initially |
Position |
After the exercise |
||
|
|
X ± m |
X ± m |
p |
X±m |
p |
|
Vs, cm/s |
-14.4 ± 1.4 |
-16.0± 1.8 |
n/d |
-15.6 ± 1.6 |
n/d |
|
VA, cm/s |
-4.5± 1.4 |
-10.2 ± 1.2 |
* |
-6.8 ± 0.9 |
n/d |
|
HR, c.u. |
78.5 ± 2.9 |
112.8±4.3 |
** |
84.3 ± 4.3 |
n/d |
The general renal and surface cortical blood flow is known to be regulated by the sympathetic nerves, and their stimulation caused arteriospasm in these regions [4]. It is clear that tachycardia during exercise could be induced by increased sympathetic influences that also involved the kidneys. According to the data presented in [5], the decreased vagal effects on the heart were accompanied by increased renal vascular resistance. However, we failed to detect arteriospasm in the kidneys because the PI and Rl parameters did not change in test subjects.

Presently, the intrarenal mechanisms of changes in the arterial blood flow parameters are rather well known. Thus, they are significantly changed in cases of renal sinus cysts and hydronephrosis [6]. The parameters of muscular activity of the arterial wall are increased in acute glomerulonephritis and during exacerbation of chronic glomerulonephritis: in acute and chronic renal failure [7-9]; with rejection of renal allograft [10-12]; in diabetic nephroangiopathia [13]; and in renal colic, especially in proximal obstruction of the ureter and signs of pyelonephritis [14]. Essential hypertension also raises the tonus of resistive renal vessels [15, 16]. A certain inconsistency of the literature data seems to be due to the different mechanisms of changes observed. In particular, at the height of renal disease blood flow in the juxtamedullar glomeruli increased along with the partially ceased blood flow in the cortex. This picture is associated with decreased PI and RI values. In more severe disease, when the juxtaglomerular apparatus is also changed and the blood cannot pass through it, the PI and Rl values again increase. This was observed in cases of irreversible damage to kidney glomeruli [17]. In stenosed renal arteries, the PI and Rl values were lower than normal [18,19].
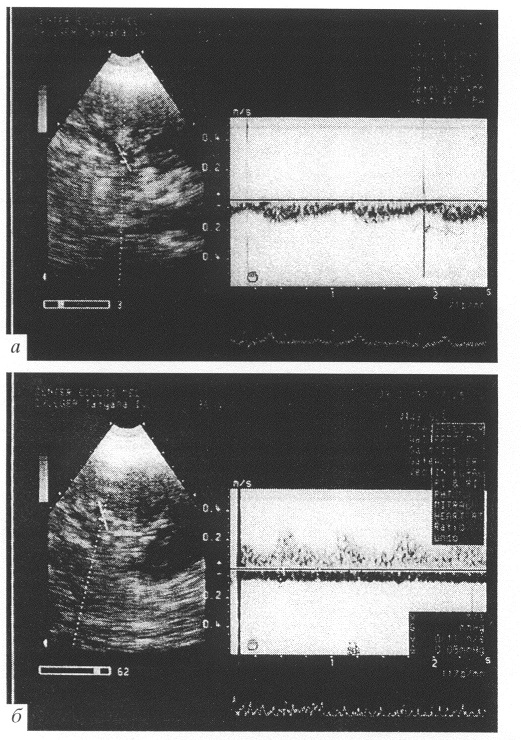
Fig. 3. Blood flow in the renal vein. (A) Betore exercise: (B) during exercise.
No changes were detected in the muscular tone of renal artery during exercise. And since the velocity parameters of the vascular blood flow correlate with the renal creatine clearance [20], it is suggested that this posture does not affect functions of the glomerular apparatus.
The increased intra-abdominal and intrarenal pressure is likely to be one of the mechanisms responsible for the effect of exercise in the cobra position on the kidneys. More than twofold-decreased cortical blood flow in the kidneys was found in dogs [21], along with an increase in the intra-abdominal pressure from 0 to 15 mm Hg. and a high correlation was found between renal blood flow and pressure in the abdominal cavity (R=0.897). In our case, the flow volume did not change in the blood vessel under observation, which suggests a relatively insignificant compression of the kidney at the backward flexure of the loins during exercise. However, it was sufficient to markedly decrease pulsations in venous outflow from the kidney due to the significantly increased blood flow during right-atrial systole (Va). and, in the more highly trained subjects, fluctuations in the venous blood flow completely disappeared when the velocity spectrum became monophase (Fig. 3).
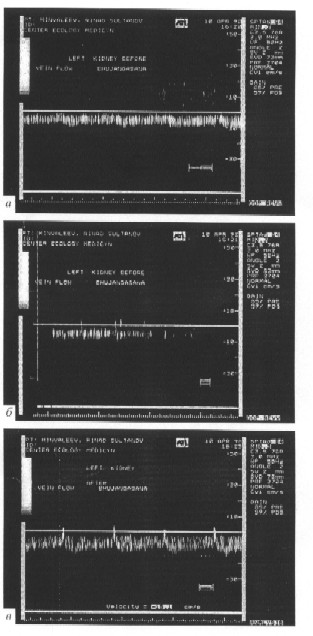
Unfortunately, the published data on the blood outflow from the kidneys are very scarce. A turbulent flow was described in the renal vein under conditions of its compression after a kidney transplantation [22]. Studies of the syndrome of compression of the left renal vein by the superior mesenteric artery and the abdominal aorta (Nutcracker syndrome) revealed a moderate decrease in the peak velocity of venous outflow in the renal hilum and a sharp acceleration of blood flow in the compressed region of the vein. No data have been reported on the minimal velocity of blood outflow from the kidney [23, 24]. Therefore, we turned to our own findings mentioned above. A monophase venous outflow was detected by the voluntary urine retention test in patients with chronic pyelonephritis complicated with pyeloureteral reflux (Fig. 6), in patients with hydronephrosis (Fig. 7), in a patient with acute ischuria because of neoplasia in the small pelvis (Fig. 8), and in the case of kidney damage associated with cirrhosis of the liver (Fig. 9). Based on the data. we suggest that disorders accompanied by the increased compression of the renal veins should result in venous outflow with either markedly smoothed fluctuations or in completely monophase outflow. And changes in this parameter preceded changes in the arterial bed that indicated the more severe damage to the kidneys.
We believe that the influence of exercise in the cobra position is within the limits of physiological fluctuations in the transmural pressure on the intra- and extrarenal blood vessels. And, naturally, the renal veins are more sensitive to such gentle effects.

Fig. 6. Blood flow in the renal vein in a patient with pyelonephritis during the voluntary urine retention test: (A) during urine retention: (B) after emptying the urinary bladder.

Fig. 7. Blood flow in the renal vein in a patient with the remaining hydronephrotic kidney after removal of the other kidney.

Fig. 8. Blood flow in the renal vein in a patient with acute ischuria caused by a voluminous process in the small pelvis.
Following the logic of our previous studies, we determined the influence of the exercise on the venous outflow from the kidneys under conditions of the initially disturbed renal blood circulation. When choosing subjects suitable for our studies, one of the yoga instructors was found to have a changed monophase blood flow in the renal vein. The changes were unilateral. The yoga exercise test was clearly positive (fluctuations in the blood flow were completely restored). Examination of the repeated dopplerograms of venous outflow after purposeful yoga exercises in the cobra position (Fig. 10) within three months showed fluctuations in the initial blood flow and its transformation into the monophase type during exercise (this indicated a correct exercise performance). After the exercise, the fluctuations increased. Some observations of this kind seem promising with respect to the favorable effects of the exercise in the cobra position on the blood outflow in the renal veins.
CONCLUSION
(1) During the exercise in the cobra position, cardiac output significantly decreases in the background of tachycardia.
(2) When the minute blood flow volume drops under the influence of exercise in the cobra position, the arterial blood supply to the kidneys remains stable.
(3) This exercise significantly increases linear flow velocity in the renal veins during right-atrial systole. and this is accompanied by a decrease or disappearance of blood pulsations in these veins.
(4) The preliminary results indicate that the initially changed venous outflow from the kidneys is restored after exercise in the cobra position.
REFERENCES
- Minvaleev R.S., Kuznetsov A.A. and Nozdrachev A.D., The Influence of Body Position on the Blood Flow of Parenchymatous Organs. 1. Liver., Fiziol. Chel., 1998. vol. 24, №4, p. 101
- Ebert D., Translated from German under the title Fiziologicheskie aspekty iogi (Physiological Aspects of Yoga), St. Petersburg. 1999. 2nd ed.
- Kuntsevich G.I., Barahashkina A.A. and Anosov. O.L., Possibilities of Duplex Scanning with Duplex-Colored Mapping in Diagnosis of Microangiopathia in Patients with Diabetes Mellitus. Vizualiz. Klin.. 1995. №7. p. 17.
- Rudenstani J., Bergstram C.J., Taghipour K. et al., Afferent Renal Sympathetic Nerve Stimulation in vivo. Effects of Regional Renal Haemodynamics in the Wistar Rat Studied by Laser-Doppler Technique, Acta Physiol. Scand., 1995, vol. 154. №3, p. 387.
- Di Carlo S.E. and Bishop V.S., Regional Vascular Resistance during Exercise: Role of Cardiac Afferents and Exercise Training, Am. J. Physiol., 1990. vol. 258 (3 Pt 2), p. 842.
- Khitrova A.N.. Dopplerography and Doppler-Colored Mapping in Differential Diagnosis of Renal Sinus Cysts and Hydronephroses. Vtoroi s’ezd Asotsiatsii spetsialistov ultrazvukovoi diagnostiki v meditsine (Second Congress of Association of Specialists in Ultrasonic Diagnosis in Medicine). Moscow, 1995. p. III.
- Dvoryakovskii I.V. and Koberidze L.Sh., Clinical Significance of Dopplerography in Nephrites in Children. Ultrazvuk. Diagnost. Akush., Ginekol.. Pediatr., 1992. №1, p. 59.
- Koruvina N.A., Al’bot V.V., Pykov M.I. et al., Renal Blood Flow in Glomerulonephritis in Children, Ultrazvuk. Diagnost. Akush., Ginekol, Pediatr., 1994, №4, p. 61.
- Enkina T.K., Zherebtsov F.K. and Grinev K.M., Ultrasonic Dopplerography of Renal Blood Flow to Predict the Outcome of Acute Renal Failure and Time of Its Solution, in Vtoroi s’ezd Assotsiatsii spetsialistov ultrazvakovoi diagnostiki v meditsine (Second Congr. of Association of Specialists in Ultrasonic Diagnosis in Medicine), Moscow. 1995, p. 104.
- De Gaetano A.M., Boldini G., Nanni G. et al. Noninvasive Surveillance of Allografted Kidneys by Ultrasonic Duplex Scanning, Angiology, 1989, vol. 40, №8, p. 705.
- Platova E.N., Sadovnikov V.I. and Belorusov O.S., Diagnosis ol Acute Rejection Crisis ol Renal Allograft by Dopplerography. in Kliniko-instrumental’naya diagnostika v khirurgii (Clinical and Instrumental Diagnosis in Surgery), Moscow. 1994. p. 98.
- Sadovnikov V.I., Platova. E.N., Goryainov V.A. et al., Ultrasonography in Diagnosis of Posttransplantation Renal Complications, in Kliniko-instrumental’naya diagnostika v khirurgii (Clinical and Instrumental Diagnosis in Surgery), Moscow, 1994. p. 99.
- Kuntsevich G.I., Barabashkina A.V., Kiryukhin A.V. and Kononovich Yu.K., Combined Ultrasonic Examination of Arteries in Diabetus Mellitus, in Vtoroi s’ezd Assotsiatsii spetsialistov ul’trazvukovoi diagnostiki v meditsine (Second Congr. of Association of Specialists in Ultrasonic Diagnosis in Medicine), Moscow, 1995, p. 56. 14. Toledo I.S., Martinez Berganza Asensio T., Cozcolluela Cabrejas R. et al., Doppler-Duplex Ultrasound in Renal Colic, Ear. J. Radiol., 1996, vol. 23, №2, p. 143.
- Jensen G., Bardelli M., Volkmann R. et al., Renovascular Resistance in Primary Hypertension: Experimental Variations Detected hy Means of Doppler Ultrasound. J. Hypertens., 1994. vol. 12, №8. p. 959.
- Kharlag G.V. and Smol”yaninova. N.G., Characteristics of Renal Blood Flow by Data of Ultrasonic Dopplerography in Patients with Arterial Hypertension in Chronic Renal Diseases, in Vtoroi s’cezd Assotsiatsii spetsialistov ul’trazvukovoi diagnostiki v meditsine (Second Congr. of Association of Specialists in Ultrasonic Diagnosis in Medicine), Moscow, 1995. p. 71.
- Pykov M.I., Ultrasonic Examination of Renal Blood Flow in Children, Vizualiz. Klin., 1996. №9, p.18.
- Veglio F., Francisco M., Melchio R. et al., Assessment of Renal Resistance Index after Captopril Test by Doppler in Essential and Renovascular Hypertension. Kidney Int., 1995. vol. 48. №5. p. 1611.
- At’kov O.Yu., Khanap G.V., Serlakova L.M. et al., Ultrasonic Assessment of Results of Reconstructive Surgery on Renal Arteries. Vizualiz. Klin., 1997. №11., p. 18.
- Makino Y., Ogava M., Ueda S., et al., Intrarenal Arterial Doppler Sonography in Patients with Various Renal Diseases: Correlation of Resistive Index with Biopsy Findings, Nippon Jinzo Gakkai Shi., 1992, vol. 34. №2. p. 207.
- Chiu, A.W.. Azadzoi, K.M., Hatzehristou D.G. et al., Effect of Intra-Abdominal Pressure on Renal Tissue Perfusion during Laparoscopy. J. Endourol., 1994, vol. 8, №2, p. 99.
- Yang C.W., Lee S.H., Choo S.W. et al., Early Graft Dysfunction due to Renal Vein Compression. Nephron, 1996, vol. 73, №3. p. 480.
- Stavros A.T., Sicker K.I. and Menter R.R., Color Duplex Sonography ol the Nutcracker Syndrome (Aortomesenteric Left Renal Vein Compression). J. Ultrasound Med., 1994, vol. 13. №7, p. 569.
- Kim S.H., Sicker K.J., Kim H.D. et al., Nutcracker Syndrome: Diagnosis with Doppler US, Radiology, 1996, vol. 198, №1, p. 93.
